What is Medicine 3.0?
Medicine 3.0 is a transformation in healthcare; a shift from a reactive, disease-focused model to a proactive, preventive, and personalized approach. By leveraging modern medical tools and scientific advancements, clinicians assess individual health risks and intervene early to prevent or mitigate diseases, aiming to enhance both lifespan and healthspan (the years in your life and the life in your years). While medicine 2.0 (the current model) waits until people are diseased to help them, medicine 3.0 emphasizes helping people avoid disease as much as possible in the first place.
Medicine 1.0
The concept of three different historical approaches to medicine, termed “Medicine 1.0”, “Medicine 2.0”, and “Medicine 3.0” was popularized by Dr. Peter Attia. Before modern medicine, much of ‘healthcare’ included treatments that were not based on the scientific method and often ranged from nonsensical (e.g. carrying a potato to cure rheumatism) to downright harmful (e.g. using leeches to drain “excess” blood or drilling holes in people’s skulls to relieve headaches). This was Medicine 1.0.
Medicine 2.0
From the late 1800’s until today, the scientific method became rigorously used in medicine. Tools were created that revolutionized diagnosis (e.g. CT scan and MRI), incredible drugs were developed that control and even cure disease (e.g., insulin, antibiotics, chemotherapy), and interventions were developed that save and prolong lives (e.g., coronary stents, robotic surgery). This is the period of Medicine 2.0. It has brought us extraordinary tools and treatments for everything from the simplest to most complex diseases we contract.
Medicine 3.0
As transformational as Medicine 2.0 was, it has some key gaps, and this is where the idea of Medicine 3.0 comes in. Where Medicine 2.0 is focused largely on treating disease once it’s already present, Medicine 3.0 uses the tools of modern medicine and science, and pre-emptively intervenes to prevent those diseases from ever occurring. It also focuses on taking you beyond just ‘absence of disease’ and into exceptional health.
In this new paradigm, the focus of healthcare shifts from curing disease to maintaining your good health to not only prolong your life (lifespan) but ensure you are fit and functional enough to enjoy the extra years you live (healthspan).
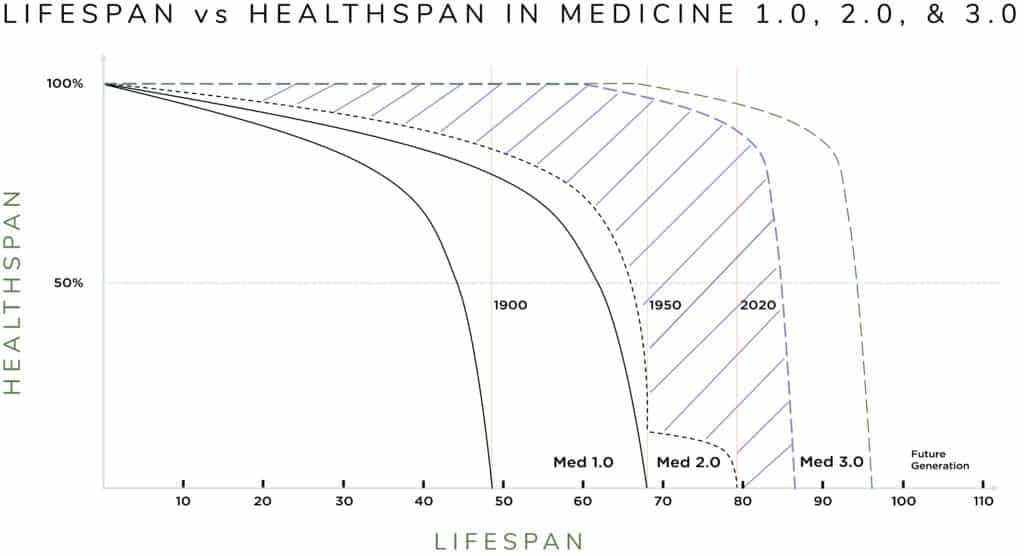
The figure below captures the difference between Medicine 2.0 and 3.0 in the purple striped area. That is, this shows the difference between ‘living longer sicker’ (Medicine 2.0) or ‘living longer with better health and functionality’ (Medicine 3.0).
In the following discussion, Dr. David Edwards and Dr. Matt McEvoy dive into this innovative paradigm, illustrating how Medicine 3.0 can lead to improved patient outcomes and a higher quality of life.
Dr. David Edwards:
My observation working as a physician in clinics, in the operating room, and rounding in the hospital is that many, if not most, of the patients I see are there because they have a disease that they were surprised by or that has finally progressed far enough that it is impossible to ignore. Whatever it is, their lives are impacted negatively, and they cannot move forward without paying attention to their health.
I’ll give an example. A kind woman I met came to see me in the pain clinic. Apparently, she had ‘bad knees’ and needed both knees replaced surgically, but she was told she was too heavy and needed to lose weight first. She had been to the weight loss clinic but did not qualify for their care or for insurance coverage for their program. Much of the weight she gained in turn came from inactivity due to her knee pain, and her arthritis worsened rapidly over this time. Now, in the pain clinic, we had to produce a plan to control the pain so that she could resume being active and qualify for surgery.
This is a typical story in the sad cycle of modern medicine. Disease (arthritis) causes impairment, results in more disease (unhealthy weight gain), and patients do not qualify for treatment until they reach a point of no return.
How should this story have played out? Well, several years earlier she could have been evaluated for strength and stability, activity, and fitness. As she aged, her body composition could have been monitored and that information used to guide activities to ensure she was able to keep her strength. When she had any signs of the onset of arthritis, training and rehabilitation potentially could have helped her avoid the disability that caused her weight spiral. She was interested in all of this information, after all, and had asked for help many times.
After learning about her goals and motivations, we decided together on some things she could do, and that I could do to help her control the pain while increasing activity. We recruited an excellent physical therapist and health coach psychologist to our cause, working as a team with her goals in mind. Over time, she was able to shed some weight, which lessened the stress and pain in her knees. She gained strength and could see progress. It has been 5 years, and she has not needed surgery to date.
I share this story, not because it demonstrates any kind of miracle or cure for arthritis, but because it is so common for the current practice of medicine to lack the time to invest early in a person’s health to prevent disease. What could have been done before disease set in, should have been done.
Dr. Matt McEvoy:
Despite the great gains of Medicine 2.0, this framework is still lacking because it is primarily reactive. Although there is a passing mention of disease prevention, the current healthcare landscape, the training in medical school and residency, and the insurance system all encourage patients to seek care only when they are sick and the treatment of disease only after it has already occurred. For instance, insurance companies will typically not approve certain medications until a person meets a lab-based criteria for being diabetic (hemoglobin A1c ≥ 6.5). However, if your A1c is 6.4, you already have damage occurring to your heart, blood vessels, nerves, kidney, eyes, and other tissues – even though you are technically pre-diabetic.
When cardiovascular disease, cancer, metabolic disease, or neurodegenerative disease have already taken hold, it can be extremely difficult (and expensive) to treat, let alone reverse. Medicine 2.0 has enabled us all to live longer (your lifespan), but it is reactive instead of proactive, so has not done as much to help us live healthy, functional lives in the last couple of decades of our lives (healthspan). In other words, modern medicine has been successful at keeping people alive longer while sick.
The figure above illustrates this idea. The vertical lines show the average lifespan in the United States in 1900 (48 yrs.), 1950 (68 yrs.), and 2020 (79 yrs.). It shows an impressive lengthening of lifespan, much of which is due to Medicine 2.0. However, if you look at the curves on the graph, they also demonstrate the concept of healthspan, which is not only how long you live, but also how healthy and functional you are as you age. The black dotted line shows that with Medicine 2.0 the lifespan is longer, but that final decade is low, meaning people are living longer while sick with less functionality. This is the aging grandparent that you think of who is alive, but who is increasingly unable to do the things that they would like, and even unable to do the most basic activities of daily living for themselves (shopping, cooking, cleaning, etc.).
This is where the idea of Medicine 3.0 comes in. It is where clinicians use the tools of modern medicine and science to determine an individual’s potential risk of getting a disease and then pre-emptively intervene to prevent development of the disease or at least greatly reduce the impact of the disease as you age. In this new paradigm, the focus of healthcare becomes maintaining your good health to not only prolong your life (lifespan, longevity health) but ensure you are fit and functional enough to enjoy the extra years you live (healthspan, wellness). In the figure, this is the difference between the curves shown by the diagonal lines. This is the goal of Medicine 3.0, personalizing medicine to prevent disease and maintain health. In other words, by investing in cardiovascular, metabolic, neurocognitive, physical, and emotional health now, people can reap the rewards into their 70s, 80s, and even 90s and beyond! Simply put, the goal is to add years to your life and health to your years.