Dr. David Edwards:
“My observation working as a physician in clinics, in the operating room, and rounding in the hospital is that many, if not most, of the patients I see are there because they have a disease that they were surprised by or that has finally progressed far enough that it is impossible to ignore. Whatever it is, their lives are impacted negatively, and they cannot move forward without paying attention to their health.
I will give an example. A kind woman I met came to see me in the pain clinic. Apparently, she had ‘bad knees’ and needed both knees replaced surgically, but she was told she was too heavy and needed to lose weight first. She had been to the weight loss clinic but did not qualify for their care or for insurance coverage for the weight loss program. She told me that much of the weight she gained in the last 2 years was due to not being active due to knee pain, and the arthritis had worsened rapidly over this time. Now, in the pain clinic, we had to produce a plan to control the pain so she could resume being active and qualify for surgery.
This is a typical story in modern medicine where disease (arthritis) causes impairment, results in more disease (unhealthy weight gain), and patients do not qualify for treatment until it reaches a point of no return. What a sad cycle this is.
How could this story have played out better for her? Well, several years earlier she could have been evaluated for strength and stability, activity, and fitness. As she aged, her body composition could have been monitored and that information used to guide maintenance activities to ensure she was able to keep her strength. When she had any signs of the onset of arthritis, training and rehabilitation potentially could have helped her avoid disability that caused her weight spiral. She was interested in all of this information, after all, and had asked for help many times.
After learning about her goals and motivations, we decided together some things she could do, and that I could do to help her control the pain while increasing activity. We recruited an excellent physical therapist and health coach psychologist to our cause, working as a team with her goals in mind. Over time, she was able to shed some weight, which lessened the stress and pain in her knees. She gained strength and could see progress. In the end, she no longer needed the surgery so urgently. It has been 5 years, and she has not needed surgery yet.
I share this story, not because it demonstrates any kind of miracle or cure for arthritis, but because it is so common for the current practice of medicine to lack the time to invest early in a person’s health to prevent disease. What could have been done before disease set in, should have been done.
I will turn it over to Dr. Matt now, to explain what this all has to do with Medicine 1.0, Medicine 2.0, and Medicine 3.0, terms popularized by Dr. Peter Attia.”
Dr. Matt McEvoy:
“As Dr. David noted, several notable figures, including Dr. Peter Attia, Dr. Andrew Huberman, and others have popularized the concept of Medicine 3.0. But that may leave you wondering, what are Medicine 1.0 and 2.0? Before the advent of modern medicine, physicians and other healthcare providers used treatments that may or may not have been helpful or tested in a scientific manner (pre-1900’s medicine). For instance, George Washington died in December of 1799 from acute epiglottitis (an infection in his throat) that could have been treated easily in modern healthcare. Instead, the doctors prescribed blood lettings (removing about half of his blood volume, 2.5 liters!) and a mixture of sage tea, vinegar, and butter. This was Medicine 1.0, an approach based on thinking, before the development of the scientific method for rigorous research. From the late 1800’s until today, the application of the scientific method has led to the development of tools that have revolutionized medical diagnosis (e.g., CT scans, MRI, angiography), incredible pharmaceuticals that control and even cure disease (e.g., insulin, antibiotics, chemotherapy), and interventions that save and prolong our lives (e.g., coronary stents, robotic surgery). This is the period of Medicine 2.0, where we have amazing tools and treatments for many of the simplest and even the complex diseases we contract.
Despite this, the framework of Medicine 2.0 is still lacking because it is primarily reactive. Although there is a passing mention of disease prevention, the current healthcare landscape, the training in medical school and residency, and the insurance system all encourage patients to seek care only when they are sick and the treatment of disease only after it has already occurred. For instance, insurance companies will typically not approve certain medications until a person meets a lab-based criteria for being diabetic (hemoglobin A1c ≥ 6.5). However, if your A1c is 6.4, you already have damage occurring to your heart, blood vessels, nerves, kidney, eyes, and other tissues – even though you are technically pre-diabetic. When cardiovascular disease, cancer, metabolic disease, or neurodegenerative disease have already taken hold, it can be extremely difficult (and expensive) to treat, let alone reverse. Medicine 2.0 has enabled us all to live longer (your lifespan), but it is reactive instead of proactive, so has not done as much to help us live healthy, functional lives in the last couple of decades of our lives (healthspan). In other words, modern medicine has been successful at keeping people alive longer while sick.
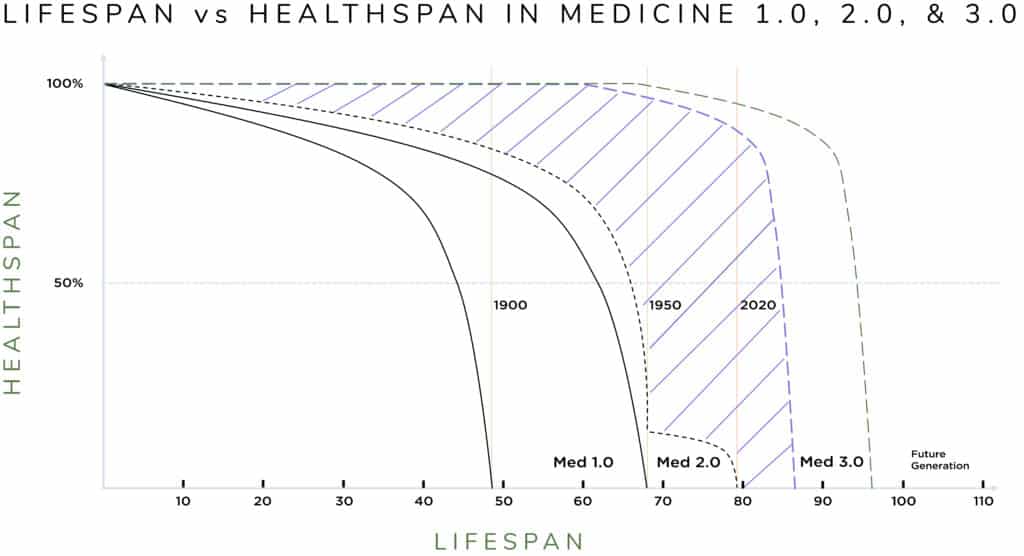
The figure in this blog illustrates this idea. The vertical lines show the average lifespan in the United States in 1900 (48 yrs.), 1950 (68 yrs.), and 2020 (79 yrs.). It shows an impressive lengthening of lifespan, much of which is due to Medicine 2.0. However, if you look at the curves on the graph, they also demonstrate the concept of healthspan, which is not only how long you live, but also how healthy and functional you are as you age. The black dotted line shows that with Medicine 2.0 the lifespan is longer, but that final decade is low, meaning people are living longer while sick with less functionality. This is the aging grandparent that you think of who is alive, but who is increasingly unable to do the things that they would like, and even unable to do the most basic activities of daily living for themselves (shopping, cooking, cleaning, etc.).
This is where the idea of Medicine 3.0 comes in. It is where clinicians use the tools of modern medicine and science to determine an individual’s potential risk of getting a disease and then pre-emptively intervene to prevent development of the disease or at least greatly reduce the impact of the disease as you age. In this new paradigm, the focus of healthcare becomes maintaining your good health to not only prolong your life (lifespan, longevity health) but ensure you are fit and functional enough to enjoy the extra years you live (healthspan, wellness). In the figure, this is the difference between the curves shown by the diagonal lines. This is the goal of Medicine 3.0, personalizing medicine to prevent disease and maintain health. In other words, by investing in cardiovascular, metabolic, neurocognitive, physical, and emotional health now, people can reap the rewards into their 70s, 80s, and even 90s and beyond! Simply put, the goal is to add years to your life and health to your years.”